Gluten Intolerance
Gluten intolerance is when you get sick after eating gluten. You might feel bloated, gassy or tired. Gluten is a protein found in many foods, especially wheat. Gluten intolerance is also called non-celiac gluten sensitivity. It’s not the same as celiac disease or a wheat allergy. About 6% of the U.S. population is gluten intolerant.
You may have a gluten intolerance if you get sick after eating gluten, a type of protein. You might feel tired, nauseous or bloated. Another name for gluten intolerance is non-celiac gluten sensitivity (NCGS).
Gluten intolerance and celiac disease are different. People with celiac disease have an autoimmune response to gluten. This means their bodies try to fight against gluten as if it were a virus. This reaction causes inflammation and damage to their digestive tracts. Celiac disease is the result of an abnormal gene. People with celiac disease also have high levels of certain antibodies in their blood, which are substances that fight gluten.
Gluten sensitivity and celiac disease cause a lot of the same symptoms. But people with gluten sensitivity don’t have an abnormal gene or antibodies in their blood.
An intolerance and a food allergy aren’t the same. A food allergy, such as a wheat allergy, is when your immune system overreacts after you eat a certain food. An allergy might cause itching, vomiting or shortness of breath. Gluten intolerance isn’t an allergy to gluten.
Your healthcare provider carefully reviews your symptoms and medical history. If they suspect you have a gluten intolerance, these are the next steps to confirm the diagnosis:
- Step 1: You eat a diet containing gluten for about six weeks. During this time, your healthcare provider performs blood tests and skin tests to rule out a wheat allergy or celiac disease. There isn’t a gluten intolerance test.
- Step 2: If you don’t have a wheat allergy or celiac disease, your healthcare provider will ask you to exclude gluten from your diet for at least six weeks. Keep a thorough record of your symptoms during this time, noting which (if any) symptoms improve.
- Step 3: If your symptoms do improve while you’re on a gluten-free diet, you gradually reintroduce gluten back into your diet. If symptoms return, you likely have a gluten intolerance.
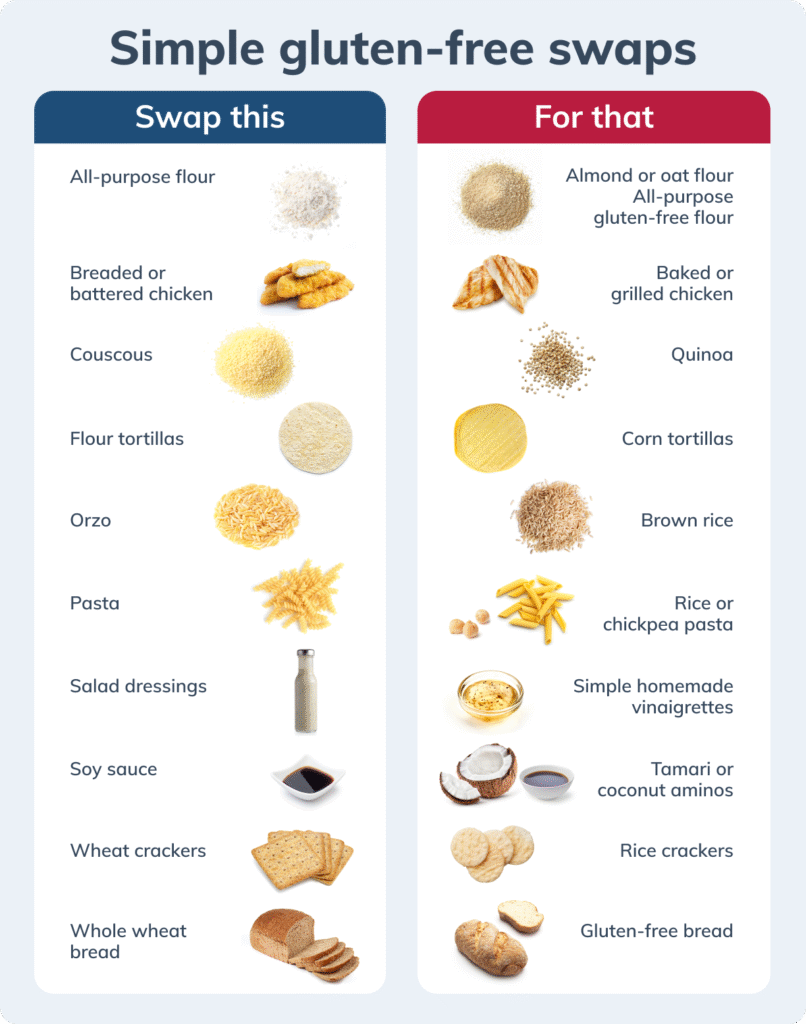
There’s no cure for gluten intolerance. But most people find relief from symptoms by following a gluten-free diet. You should work with your healthcare provider and a dietitian to plan your diet.
You can also ask your healthcare provider about adding probiotics to your diet. Probiotics help increase the good bacteria in your gut. They may reduce symptoms of bloating, gas or constipation.
Some research suggests that taking certain enzymes may help you digest gluten. But experts are still investigating this treatment. Talk to your healthcare provider before taking any enzymes.
There’s no way to prevent gluten intolerance, but there are ways to reduce the symptoms. Talk to Rodeynurse about a treatment plan that works for you.
https://rodeynurse.intakeq.com/booking
Reference
https://my.clevelandclinic.org/health/diseases/21622-gluten-intolerance
https://fs-marketing-files.s3.amazonaws.com/infographics/gluten-free-swaps.png